|
FOOD PSYCHOLOGY Daniel Roberts, Ph.D. & Brenda MacDonald, M.Ed. Stress, Diet, and Disease Summary: Stress per se and stress-related foods lead to excessive secretions of corticosteroid hormones in the blood stream. Cortisol, especially, affects an individual's functioning ability and well-being. Long-term, sustained high cortisol levels has negative effects on health and promotes chronic disease. Particularly, sugar-laden foods causing excessive release of cortisol put people on a sugar 'load' roller coaster that has similar biophysiological effects as stress on the brain's structures and the internal organs served by the autonomic nervous system. In particular, both stress and diets high in sugar content increase cortisol levels and the likelihood of endocrine imbalance that takes a major toll on the organ's systems. To stop the harmful side-effects of a high-sugar diet, one has to revert to a healthier diet, and stop, or reduce the consumption of high-sugar products. However, sugar is an addictive substance triggering the release of dopamine that stimulates the brain's pleasure centers. On the positive side, individuals with specific personality characteristics (e.g., an internal locus of control and a positive attitude) are better able to fend off stress. It is expected that people who switch to a healthier diet, and adopt stress-moderating traits through cognitive restructuring, will acquire personality-related mindsets leading to more healthy habits. As well, relaxation, mindfulness, and other meditative techniques have been shown to counter the effect of cortisol stemming either from stress or high-sugar foods. Importantly, stress-related foods do not facilitate rational or intellectual activity. However, as we move away from stress-related brainwaves (i.e., beta waves), to more alpha brainwaves, we become more able to intellectually nurture our thoughts, and focus on achieving personal goals. Overall, a healthier diet along with stress-reducing moderators is most likely to lead to a healthier lifestyle, including better health, and longevity.
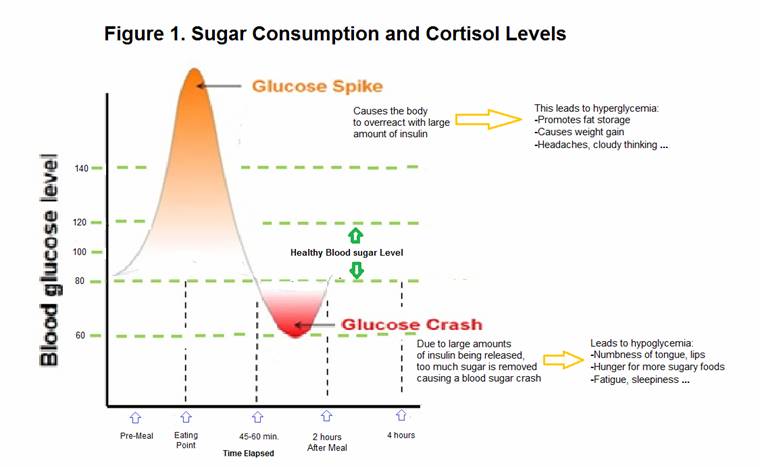
Much like research on stress, evidence has accumulated showing that patterns of nutrition (eating habits) influence an individual's susceptibility to a variety of psychological and physical diseases. Of course, nutritional habits interact with other factors, such as psychological, genetic and the social-environmental. Nonetheless, it is well established that food habits influence the functioning of the brain and that of the body's internal organs, particularly those served by the autonomic nervous system, thereby increasing the susceptibility to chronic disease. In particular, research findings show that adults exposed to high stress levels and/or a diet high in sugar have a higher probability of developing a broad array of chronic disorders, such as cardiovascular disease, arthritis, hypertension, and immune-related deficiencies (Glaser & Kiecolt-Glaser, 2009; Jemmott & Locke, 1984; Segerstrom & Miller, 2004; Stojanovich & Marisavljevich, 2008). Selye (1976) developed the concept of the General Adaptation Syndrome to describe the biophysiological changes that occur when a person experiences undue stress. The general adaptation syndrome, or more simply, the stress response, consists of three phases. In the first phase, that of alarm, the organism becomes mobilized to meet the threat. In the second phase, resistance, the organism makes efforts to cope with the threat. The third phase, exhaustion, occurs if the organism failed to overcome the threat and depletes its physiological resources in the process of trying. Eventually, exhaustion leads the organism to experience hormonal exhaustion, although the core of the problem is the chronic overactivation of the stress response which has damaging physiological effects on a variety of organ systems; e.g., cardiovascular, endocrine, nervous, and digestive systems. The origins of stressors Selye (1974) wrote that stressful stimuli take a variety of forms; these can range in severity, from micro-stressors (i.e., the daily hassle of everyday annoyances) to severe stressors, such as major negative events. H identified psychological stressors (such as divorce, moving residence and death of a loved one), and physical stressors (such as alcohol and drug abuse, smoking, and illness) that elicit the body's stress response. Anisman and Merali (1999) distinguished stressors in terms of whether they are psychogenic or neurogenic. Psychogenic stressors originate from psychological factors (e.g., anticipation of an adverse event), while neurogenic stressors stem from a physical stimulus (e.g., bodily injury or recovery from injury). In this context, an unhealthy diet, or excessive use of substances such as sugar and fat that harm the functioning of body's organs, leading to chronic conditions, are considered stressors. It is important to point out that though stress per se, and sugar, have similar biophysiological effects on the body's organs, psychologically, however, there are some differences. Sugar gives us a jolt of 'feeling good', while worries precede stress. On the other hand, eustress or positive stress gives us a feeling of fulfilment and other positive feelings. Sugar is addictive, but stress can also be addictive and, at high levels become detrimental to one's health and well-being. Indeed, some personality types feed on an 'adrenaline high' (i.e., stress). McAndrew (2018) and many other researchers (e.g., Dimitru & Cozman, 2012; Mecacci & Rocchetti, 1998; Sinha, 2018) have documented personality traits associated with unhealthy diets, and damaging high-stress levels. Exposure to stress hormones Current research shows that a diet high in sugar content stimulate the body to release stress hormones; e.g., cortisol. For instance, when we eat something sugary, like a chocolate bar and have a soft drink with it, our blood sugar will spike quickly, and then come crashing down just as quickly because in response to the sugar, the body releases insulin, the hormone that stores the sugar (glucose and fructose) in the cells. The up and down of high sugar levels in the bloodstream is sometimes referred to as sugar 'loads'. Sugar loads have the same reward areas in the brain as nicotine and cocaine. However, the sugar 'rush' does not last long and, to re-establish this 'happy feeling', our brain will signal us to eat something sweet again, so that we can 'feel good' again (Figure 1). From the spikes and crashes of this sugar roller coaster, emerges the problem with adrenaline that leads to cognitive problems, such as short attention, difficulty with concentration, and headaches. Importantly, in the long run, eating excessive amounts sugar is a leading cause of damage to our internal organs which, in turn, lead to a multitude of physical illnesses, such as heart-related diseases, type-2 diabetes, and immune-related conditions.
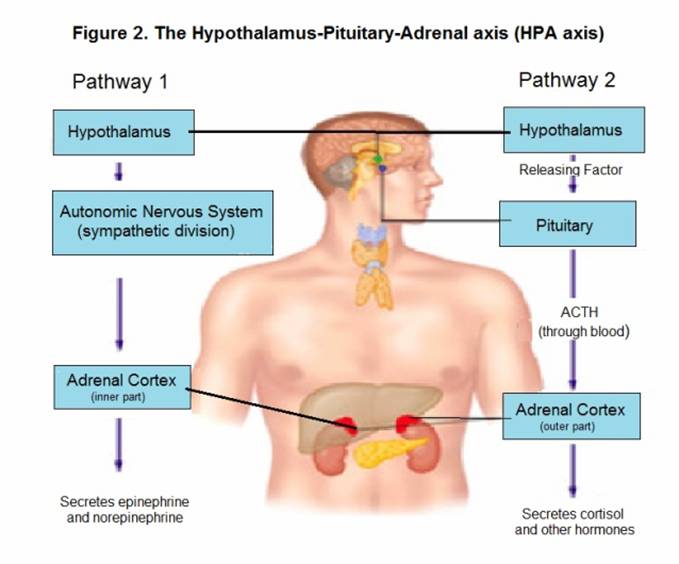
The American Heart Association (AHA) recommends no more than 6 teaspoons (25 grams) of added sugar per day for women and 9 teaspoons (38 grams) for men. One teaspoon is roughly equivalent to 4 grams of sugar. However, people in western countries eat 20 teaspoons. Moreover, most people consume as much as 2300 calories a day including more than 30 teaspoons of sugar. Asking people to abide by the AHA's guidelines is easier said than done because sugar is an addictive substance. Mounting research indicates that a diet high in sugar influences the brain's dopamine reward system. In addition, the continued consumption of a sugary diet that leads to chronic stress suppresses the reward system (so people would find less enjoyment). One of the findings in the literature on energy is that the more one eats sugar-laden food, the more he/she will desire food with high sugar content. McEwen's model (1998) describes what happens during exposure to stress hormones (Figure 2). He theorized that when under stress, the hypothalamus sends messages to the endocrine glands via two major pathways. The first pathway is embedded in the autonomic nervous system: it stimulates the central part of the adrenal glands (the adrenal medulla) to release large amounts of catecholamines (e.g., epinephrine and norepinephrine) into the bloodstream. These hormones produce the physiological changes seen in the fight-or-flight response. The second pathway is a more direct communication between the brain and the endocrine system. Here, the hypothalamus sends signals to the anterior part of the pituitary, which then secretes a hormone (ACTH) that stimulates the outer part of the adrenal cortex to release corticosteroids. Short-term, people's reactions to the biological changes resulting from stressors are adaptive; it can enhance immuno-protection, as well as mental and physical performance (Dhabhar, 2018). Long-term, however, the persistent activation of the Hypothalamic-Pituitary-Adrenal axis (HPA) has significant detrimental effects. The repeated activation of the HPA axis in response to chronic secretion of cortisol has shown to compromise the functioning of the HPA axis. When the HPA axis becomes dysregulated, daily cortisol patterns can be altered, leading to the classical effects of cortisol on the body's organs, especially those of the brain's limbic structures (e.g., the hippocampus) and the internal organs under control of the autonomic nervous system.
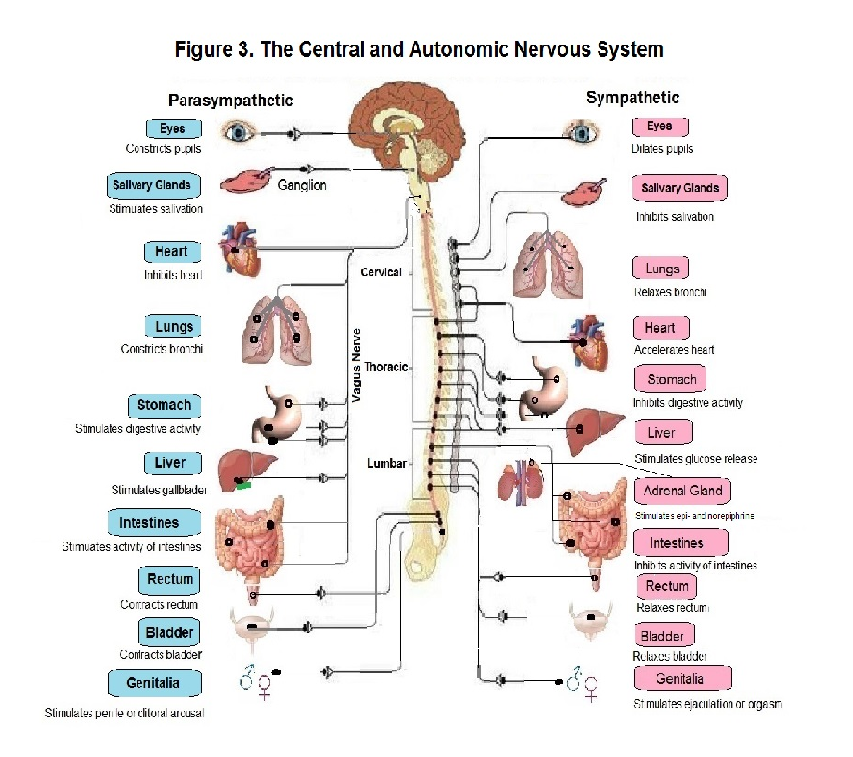
Normally, cortisol is high upon waking in the morning, decreases over the day (although peaking following lunch), until it flattens out with low levels in the afternoon, becoming lowest in the evening, when preparing for sleep. However, people under chronic stress or under the effects of stress-inducing foods can have elevated cortisol levels long into the afternoon or evening (Powell et al., 2002), a general flattening of the diurnal rhythms and an exaggerated cortisol response or, alternately, no response. Any of these responses following elevated cortisol levels can compromise the ability of the HPA axis to respond to and recover from either stress or stress-related foods; that is, for an individual to go back to a homeostatic state: i.e., a state of equilibrium where he/she can maintain an internal environment in which brainwaves are best suited for thinking and decision-making, as well as a healthy circadian rhythm that promotes consistent and restorative sleep. It should be pointed out that perceived stress leads people to eat energy foods that are high in sugar. Also, either stress or stress-related foods lead to sugar cravings. As well, long-term consumption of high sugar diets cause people to eat more of a high sugar diet because of withdrawal symptoms or the sugar 'rush' wearing off. The switch from a hyper-vigilant state (of being alert and concentrated) to a sluggish state of mind can be unpleasant. For instance, an individual can have feelings of vagueness and of being aloof and sluggish. Some have labelled this state a 'sugar hangover', where fatigue and headaches are common. As well, people have experienced anxiety, anger, and aggression during sugar withdrawal. The Autonomic Nervous System The Autonomic nervous System (Figure 3) is subdivided into the sympathetic nervous system and the parasympathetic nervous system. The function of the Autonomic Nervous System (ANS) is to regulate the body's automatic, involuntary functions. A characteristic of the ANS is the nerve's synapse: a cluster of nerves called a ganglion where a message goes through before being transmitted to the target organ. The nerves from the Central Nervous System (CNS) to the ganglion are known as preganglionic nerves. The nerves of the preganglionic parasympathetic nervous system arise in the CNS and include several cranial nerves as well as three pelvic nerves. These preganglionic nerves release acetylcholine at their synapses. The sympathetic preganglionic neurons have dendrites and cell bodies in the grey matter of the thoracic and upper lumbar segment of the spinal cord. Cortisol is one of its main neurotransmitters. The sympathetic nervous system serves to regulate and modulate unconscious actions primarily related to the fight-or-flight response. The sympathetic nervous system, when activated, accelerates the heartbeat, and initiates other smooth-muscle and glandular responses. On the other hand, the parasympathetic nervous system is involved in deactivation and the restoration of the organism to a lower state of activation: it lowers blood pressure and heart rate. It also stimulates bodily functions, such as increasing muscular activity of the stomach and intestines. When its neurotransmitters are at appropriate levels, the brain functions harmoniously and the overall mood is one of well-being.
Cortisol-induced conditions A variety of internal organs innervated by the autonomic nervous system (ANS) has been established as an indirect cause or an important risk factor in a multitude of conditions. This is the case for stress-related and food-induced disease. Indeed, the excessive secretions of stress-related hormones (e.g., cortisol), either due to emotional/physical stress or a diet high in sugar content, were reported to have similar effects on individuals' cognitive and bodily functions. For example, high cortisol levels has been shown to cause a large number of symptoms. General signs and symptoms of high cortisol concentrations include weight gain, muscle weakness and fatigue, irritability, high blood pressure, headaches, and difficulty concentrating (Dowlati et al, 2010; DiNicolantonio et al., 2018; Matthew et al, 2015; Simmons et al., 2010). The excessive secretion of cortisol also has a negative effect on mitochondrial functioning (Gvozdjakova, 2008). For instance, mitochondrial dysfunction is involved in chronic inflammation and excessive pruning (the destruction of live neurons), which, eventually, leads to problems in verbal functioning and cognitive dysfunctions (Starkman et al., 2001; Wingerfeld & Wolf, 2014; Dienstbier, 2015). Also, since stress acts at the brain level through the hypothalamic-pituitary-adrenal glands, it can suppress the activity of bone growth and that of female and male reproductive organs, inhibiting reproduction (Alam et a., 2020; Massey et al., 2016; Whirledge & Cidlowski, 2010). Moreover, the stress-related hormones cause epigenetic changes; it was found that chronic exposure to high levels of cortisol causes modifications both to the epigenome and DNA, prompting changes in gene expression (Black et al., 2016; Flaherty et al., 2017; Provençal & Binder, 2015). Stress and heart disease The high cortisol levels from either high stress or a poor diet makes people at greater risk for developing coronary heart disease. Over the long-term, over-consumption of sugar and overproduction of stress-related hormones, associated with repetitive stress levels, produces hemodynamic changes, such as increased blood pressure, which eventually disposes people to atherosclerosis; shrinking and clogging of the arteries, heart attacks, and strokes (Matthews & Gump, 2002, Smith et al., 2005; Taylor, 2009). Other diets also increase the risk for chronic diseases. For instance, diets high in fat are at the source of biophysiological changes which not only lead to cardiovascular diseases, but also diseases of the digestive, and immune systems (Skeaf & Miller, 2009). In the case of high fat diets, however, the biophysiological mechanisms, by which high fat consumption damages the body's organs, such as the heart, or pancreas, leading to diabetes, are different from stress or a sugar-laden diet. One research finding, for example, point to host cells being damaged, especially cells of the intestinal epithelium. The intestinal epithelium plays a crucial role in modulating the function of the intestinal flora; it can ‘turn on’ or ‘turn off’ metabolic pathways in the microbes that directly affect the risk for certain diseases, including immune disease, diabetes, and heart disease. Stress and the immune system The immune system consists of cells that protect the body from environmental agents such as bacteria and viruses, thereby preserving the integrity of the body. When a body is functioning on high cortisol levels, it can lead to suppression of the immune system, particularly the cellullar immune functions that protects against infectious diseases. Normally, where the immune system responds to infection or injury, it releases proinflammatory cytokines. It is well documented that cytokines are proteins that orchestrate a number of immune activities that play a role in killing the pathogens and repairing damaged tissue. However, exposure to long-term stress and/or a diet high in sugar content leads to persistent overproduction of proinflammatory cytokines, and chronic inflammation, which contributes to disease, such as arthritis, osteoporosis, cold, flu, and upper respiratory infections (Christian et al., 2009; Glaser, & Kiecolt-Glaser, 2005; Kiecolt-Glaser et al., 2002). Cortisol and type 2 diabetes Often associated with heart diseases and immune related disorders is type 2 diabetes. Higher cortisol levels have been associated with a decrease in beta cell function in the pancreas and increased levels of hemoglobin-A-1c (Di Damalzi et al, 2012; Joseph & Golden, 2016; Sharma & Singh, 2020). As in other cortisol-related diseases, changes were observed in the Hypothalamus-Pituitary-Adrenal axis, as were alterations in the gut intestinal flora, and atrophy of the hippocampus. Common symptoms include low energy, brain fog, and mood swings. Infections are also more common in people with diabetes because immune function is lower, which can lead to systemic infections such as the cold or flu, or local infections such as ulcerated feet or tooth infections. Moderators of stress, and disease How people respond to stress is substantially influenced by their learning history, gender, personality, intelligence, socioeconomic status, social resources, and genetic predisposition. For instance, individual differences have been linked to variations in stress and coping style, social support and resilience, health, social standing, and longevity. One factor that influences vulnerability to stress is optimism; a tendency to have a favourable, constructive view of situations and to expect positive outcomes. Scheier and Carver (1987, 1992) found a correlation between optimism and good physical health. Other studies have found optimism to be associated with more effective immune functioning (Segerstrom et al., 2007; Segerstrom & Sehpton, 2010). Moreover, in a study involving a large cohort of male participants, optimists had a lower incidence of coronary heart disease than did pessimists (Kubzansky et al. 2001). In yet another study, optimism was linked with better mental health (Achat et al., 2000). Similarly, researchers at the Mayo Clinic administered personality tests assessing optimism and pessimism in patients who came into the clinic for general medical issues during the 1960s. Thirty years later, the data on optimism and pessimism were compared with patient survival. The researcher found a 19% increase in mortality risk in people who were consistently pessimistic (Maruta et al 2000). A health factor related to optimism is an internal locus of control. People with an internal locus of control are more likely to avoid a risky lifestyle that involves health-compromising behavior (Chang, 1998). In general, locus of control refers to our expectation about whether we can control the things that happen to us (Rotter, 1990). People who have an internal locus of control tend to believe that they are responsible for what happens to them, and that they control their own destiny. On the other hand, people who have an external locus of control tend to believe that their lives are controlled by luck, fate, or other people. An internal locus of control has been associated with many aspects of life, including health, academic achievement, political activism and emotional well-being (Lang & Heckhausen, 2001; Marshall, 1991; Strickland, 1989). Closely linked to the concept of optimism are positive emotions. People who experience more positive emotions have a positive attitude; they have a tendency to perceive situations in a positive way and are also more likely to find positive elements in situations. In contrast, pessimists tend to have a negative perception of life and expect negative outcomes. Negative emotions, such as resentment, regret, and worry, usually keep the body's biological system aroused and the body in a continuous state of emergency, sometimes for longer than it can tolerate (Avey, Wernsing & Mhatre, 2011; Cohn & Fredrickson, 2009; A longitudinal study was carried out with a group of females having a nearly identical lifestyle: nuns. The Nun Study allowed researchers to examine how personality factors affected people over the course of their lifetime while controlling for variables such as diet, world demands, and stress. The handwritten autobiographies of 180 nuns were analyzed; these documents were written by the nuns when they were entering the order in their early-to-mid twenties. A strong correlation was reported between positive emotions during young adulthood and the longevity of the nuns--nuns or people who were more positive during their twenties lived longer than less positive people (Danner et al., 2001). People's personality, cognitive, and emotional characteristics are important contributors to resiliency. A concept related to resilience is hardiness. Whereas hardiness refers to characteristics that help one cope with stress, resilience refers to recovery, or positive growth following stress, including after extreme adversity (Bonnano et al, 2007). Holocaust survivors were resilient people. One survivor of a concentration camp stated that he would not have the oppressors control his emotions; this attitude made him less vulnerable to atrocities. In general, a resilient personality has the ability to effectively recover from illness or adversity. Resilient people have several factors in their favour; a constellation of traits that determine how they perceive, think about, and relate to themselves and the environment. Resilient people also have more complex organizing and integrative systems that include cognitive and emotional components (Ong, Bergeman & Chow, 2010; Skodol, 2010). Strategies for healthier a lifestyle Undoubtedly, high-sugar foods and diets have innumerable side-effects impacting on an individual's health and well-being. However, there are evidence-based practices—including dietary and lifestyle changes—that can help. Since sugar increases cortisol levels in the bloodstream, refined sugar or food high in sugar content are to be limited or cut out. Switching to a healthy diet is most important. That's because a poor diet can actually cause an unhealthy response to stress. Eating a diet that falls short of vital nutrients can contribute to stress, tiredness as well as the development of health problems, and chronic diseases. Therefore, a sound nutritional plan provides the right amount of all the nutrients we need: carbohydrates, proteins, fat, vitamins, minerals and water. Good nutrition helps channel stress effectively and, also, shape better eating habits. Stress is a trigger for high-sugar foods. And, vice versa, a diet high in sugar is conducive to stress. In either case, research has shown high elevations of stress hormones, including cortisol. The additive effects of a an unhealthy diet or/and stress speeds up the process of wear and tear, causing ever greater damage to the body's systems, and organs. Adding anxiety to the mix rapidly worsen the problem. Anxiety is an overreaction in the first stage of the body's stress response. When the first phase of the stress response becomes exaggerated, especially among worriers, it becomes a source of anxiety, illness, and will very likely shorten one's lifespan, or longevity. Cognitive Behavioral Therapy (CBT) was found effective in stress-like conditions that are associated with high cortisol levels. Adopting the mindsets that underlie personality traits moderating stress can lead to adaptive change. These traits associated with respective mindsets (the sets of beliefs and thoughts that make up one's mental attitude, and his/her interpretations and responses to events, circumstances and situations) are associated with lifestyles related to health, longevity, and social status. Using relaxation, mindfulness, Yoga and other meditative techniques can help us think and reason more clearly. The increased production of cortisol associated with high-range beta frequencies does not facilitate decision-making or intellectual activity. A lack of rational thinking makes us less able to think of solutions to deal with stress-related challenges. However, in a meditative state which decreases cortisol levels and supports healthy neurochemistry, our brain moves into an alpha state. This is a relaxed and alert condition that allows us to think more clearly. An alpha brain allows us to be attentive and focused. Intellectually, we are more able to nurture dietary choices, exercise, plan for the future and, especially, find solutions towards maintaining our life goals (Hardt, 2020; Kamei, Toriumi & Kimura, 2000; van Peer, Roelofs & Spinhoven, 2008; Wells, 2021).
References Achat, H., Kawachi, L., Spiro, A., DeMolles, D. A., & Sparrow, D. (2000). Optimism and depression as predictor of physical and mental health functioning: The Normative Aging Study. Annals of Behavioral Medicine, 22, 127-130. http://doi:10.1007/bf02895776 Alam, F., Khan, T. A., Ali, R., Tariq, F., & Rehman, R. (2020). SIRTI and cortisol in unexplained infertile females; a cross sectional study, in Karachi Pakistan. Taiwanese Journal of Obstetrics and Gynecology, 59(2), 189-194. http://doi:10.1016/j.tjog.2020.01.004 Anisman, H., & Merali, Z. (1999). Understanding stress: Characteristics and caveats. Alcohol Research and Health, 23, 241-249. Avey, J. B., Wernsing, T. A., & Mhatre, K. H. (2011). A longitudinal analysis of positive psychological constructs and emotions on stress, anxiety, and well-being. Journal of Leadership & Organizational Studies, 18(2), 216-228. https://doi.org/10.1177/1548051810397368 Black, C. N., Bot, M., Révész, D., Scheffer, P. G., & Penninx, B. (2017). The association between three major physiological stress systems and oxidative DNA and lipid damage. Psychoneuroendocrinology, 80, 56-66. http://doi.10.1016/j.psyneuen.2017.03.003 Bonnano, G. A., Galea, S., Buciarelli, A., & Vlahow, D. (2007). What predicts psychological resilience after disaster? The role of demographics, resources, and life stress. Journal of Consulting and Clinical Psychology, 75(5) 671 682. http://doi..1037/0022-006x.75.5.671 Chang, E. C. (1998). Dispositional optimism and primary and secondary appraisal of a stressor: Controlling the confounding influences and relations to coping and psychological and psychical adjustment. Journal of personality and Social Psychology, 74(4),1109-1120. https://doi.org/10.1037/0022-3514.74.4.1109 Christian, L. M., Franco, A. Glaser, R., & Lams, J. D. (2009). Depressive symptoms are associated with elevated serum proinflammatory cytokines among pregnant women. Brain, Behavior, and Immunity, 23(6), 750-754. https://doi.org/10.1016/j.bbi.2009.02.012 Cohn, M. A., & Fredrickson, B. L. (2009). Positive emotions. In C. R., Snyder & S. J. Lopez. The Oxford Handbook of Positive Psychology (2nd ed., pp. 12-24) Oxford University Press. https://doi.org/10.1093/oxfordhb/9780195187243.013.0003 Dhabhar, F. S. (2018). The Short-Term Stress Response – Mother Nature’s Mechanism for Enhancing Protection and Performance Under Conditions of Threat, Challenge, and Opportunity. Frontiers in Neuroendocrinology, 49, 175-192. http://doi:10.1016/j.yfrne.2018.03.004 Danner, D. B., Snowdon, D. A., & Friesen, W. V. (2001). Positive emotions in early life and longevity: Findings from the nun study. Journal of Personality and Social Psychology, 80(5), 804-813. https://doi.apa.org/doi/10.1037/0022-3514.80.5.804 Di Dalmazi, G., Pagotto, U., Pasquali, R., & Vicennati, V. (2012). Glucocorticoids and Type 2 Diabetes: From Physiology to Pathology. Journal of Nutrition and Metabolism, Volume 2012. https://doi.org/10.1155/2012/525093 Dienstbier, R. A. (2015). Long-term Stress: Stress Kills Neurons Too. Building Resistance to stress and aging, 85-94. https://doi.org/10.1057/9781137454850_7 Dimitru, V. M., & Cozman, D. (2012). The relationship between stress and personality factors. Human and Veterinary Medicine, 4(1), 34-38. https://www.researchgate.net/publication/268063280_The_relationship_between_stress_and_personality_factors DiNicolantonio, J. J., Mehta, V., Onkaramurthy, N., & O'Keefe, J. H. (2018). Fructose-induced inflammation and increased cortisol: A new mechanism for how sugar induces visceral adiposity. Progress in Cardiovascular Diseases, 61(1), 3-9. http://doi.10.1016/j.pcad.2017.12.001 Dowlati, Y., Herrmann, N., Swardfager, W. Thomson, S., Oh, P. I., Van-Uum, S. V., Koren, G., & Lanctot, K. (2010). Relationship between hair cortisol concentrations and depressive symptoms in patients with coronary artery disease. Neuropsychiatric Disease and Treatment. 6, 393-400. http://doi.10.2147/ndt.s10353 Flaherty, R. L., Owen, M., Fagan-Murphy, A., et al. (2017). Glucocorticoids induce production of reactive oxygen species/reactive nitrogen species and DNA damage through an iNOS mediated pathway in breast cancer. Breast Cancer Research, 19(35). https://doi.org/10.1186/s13058-017-0823-8 Glaser, R., & Kiecolt-Glaser, J. (2005). Stress-induced immune dysfunction: Implications for health. Nature Review Immunology, 5, 243–251. https://doi.org/10.1038/nri1571 Gvozdjakova, A. E. (2008). Mitochondrial medicine (Mitochondrial metabolism, diseases, diagnosis and therapy. Gvozdjakova, A., Ed. Springer. https:/doi:10.1134/S1990747809020184 Hardt, J. (2020). Stress, anxiousness, and the brain wave connection. https://www.neuroscienceinc.com/news/2020/stress-anxiousness-and-the-brain-wave-connection Jemmott, J. B., & Locke, S. E. (1984). Psychosocial factors, immunologic mediation, and human susceptibility to infectious diseases: How much do we know? Psychological Bulletin, 95(1), 78–108. https://doi.org/10.1037/0033-2909.95.1.78 Joseph, J. J., & Golden, S. H. (2017). Cortisol dysregulation: the bidirectional link between stress, depression, and type 2 diabetes mellitus. Annals of the New York Academy of Sciences, 1391(1), 20-34. https://doi.org/10.1111/nyas.13217 Kamei, T., Toriumi, Y., Kimura, H., et al. (2000). Decrease in serum cortisol during yoga exercise is correlated with alpha wave activation. Perceptual and Motor Skills, 90(3). https://doi.org/10.2466/pms.2000.90.3.1027 Kiecolt-Glaser, J. K., McGuire, L., Robles, T. F., & Glaser, R. (2002). Psychological influences on immune functions and health. Journal of Consulting and Clinical Psychology, 70(3), 537-547. https://doi.org/10.1037/0022-006x.70.3.537 Kubzansky, L. D., Sparrow, D., Vokonas, P., & Kawachi, I. (2001). Is the glass half empty or half-full? A prospective study of optimism and coronary heart disease in the normative aging study. Psychosomatic Medicine, 63(6), 910-916. https:/doi.org/10.1097/00006842-200111000-00009 Lang, E. R., & Heckhausen, J. (2001). Perceive control over development and subective well-being: Differential benefits across adulthood. Journal of Personality and Social Psychology, 81(3), 509-523. https:/doi.org/10.1037/0022-3514.81.3.50 Marshall, G. N. (1991). A multidimensional analysis of internal health locus of control beliefs: Separating the wheat from the chaff? Journal of Personality and Social Psychology, 61(3), 483–491. https://doi.org/10.1037/0022-3514.61.3.483 Maruta, T., Colligan, R. C., Malinchoc, M., & Offord, K. P. (2000). Optimists vs. pessimists: Survival rate among medical patients over a 30-year period. Mayo Clinic Proceedings, 75(2), 140-143. https:/doi.org/10.1016/s0025-6196(11)64184-0 Massey, A. J., Campbell, B. K., Raine-Fenning, N., Pincott-Allen, C., Perry, J., & Vedhara, K. (2016). Relationship between hair and salivary cortisol and pregnancy in women undergoing IVF. Psychoneuroendocrinology, 74, 397-405. http://doi.10.1016/j.psyneuen.2016.08.027 Excessive Sugar Consumption May Be a Difficult Habit to Break: A View From the Brain and Body. The Journal of Clinical Endocrinology & Metabolism, 100(6), 2239–2247. https://www.doi.org/10.1210/jc.2014-4353 Matthews, K A., & Gump, B. B. (2002). Chronic Work Stress and Marital Dissolution Increase Risk of Posttrial Mortality in Men From the Multiple Risk Factor Intervention Trial. McAndrew, F. (2018). When do personality traits predict behavior. https://www.psychologytoday.com/ca/blog/out-the-ooze/201810/When Do Personality Traits Predict Behavior? | Psychology Today Canada McEwen, B. S. (1998). Protective and damaging effects of stress mediators. New England Journal of Medicine, 338, 171-179. http://doi.10.1056/nejm199801153380307 Mecacci, L., & Rocchetti, G. (1998). Morning and evening types: stress-related personality aspects, Personality and Individual Differences, 25(3), 537-542. https://doi.org/10.1016/S0191-8869(98)00087-7 Ong, A. D., Bergeman, C. S., & Chow, S. M. (2010). Positive emotions as a basic building block of resilience in adulthood. In J. W., Reich, A. J. Zautra, J. S. Hall (Eds). Handbook of adult resilience (pp. 81-93). The Guilford Press. Powell, L. H., Lovallo, W. R., Matthews, K. A., et al. (2002). Physiologic markers of chronic stress in pre-menopausal, middle-age women. Psychosomatic Medicine, 64(3), 502-509. https://doi 10.1097/00006842-200205000-00015 Provençal, N., & Binder, E. B. (2015). The effects of early life stress on the epigenome: From the womb to adulthood and even before. Experimental Neurology, 268, 10-20. https://doi.org/10.1016/j.expneurol.2014.09.001 Rotter, J. B. (1990). Internal versus external control of reinforcement: A case history of a variable. American Psychologist, 45(4), 5-37. https:/doi.org/10.1037/0003-066x.45.4.489 Scheier, M. F., & Carver, C. S. (1987). Dispositional optimism and physical well being: the influence of generalized outcome expectancies on health. Journal of personality, 55(2), 169-210. https://doi.org/10.1111/j.1467-6494.1987.tb00434.x Scheier, M. F., & Carver, C. S. (1992). Effects of optimism on psychological and physical well-being. Theoretical overview and empirical update. Cognitive Therapy and Research, 16(2), 201-228. https:/doi.org/10.1007/bf01173489 Segerstrom S. C., & Sephton, E. E. (2010). Optimistic expectancies and cell-mediated immunity: The role of positive affect. Psychological Science, 21(3), 448-455. https:/doi.org/10.1177/0956797610362061 Segerstrom S. C. (2007). Optimism and resources: Effects on each other and health over 10 years. Journal of Research in Personality, 41(4), 772-786. https://doi.org/10.1016/j.jrp.2006.09.004 Segerstrom, S. C., & Miller, G. E. (2004). Psychological Stress and the Human Immune System: A meta-analytic study of 30 years of Inquiry. Psychological Bulletin, 130(4), 601-630. http.//DOI:10.1037/0033-2909.130.4.601 Selye, H. (1976). Stress in health and disease. Butterworth Publishers Inc. Selye, H. 1974). Stress without distress. Philadelphia: W. B. Sounders. Sharma, V. K., & Sing, T. G. (2020). Chronic Stress and Diabetes Mellitus: Interwoven Pathologies. Current Diabetes Review, 16(6), 546-566. https://doi.org/10.2174/1573399815666191111152248 Simmons, J. G., Badcock, P. B., & Whittle, S. L. (2016). The lifetime experience of traumatic events is associated with hair cortisol concentrations in community-based children. Psychoneuroendocrinology, 63, 276-281. https://doi.org/10.1016/j.psyneuen.2015.10.004 Sinha, R. (2018). Role of addiction and stress neurobiology on food intake and obesity. Biological Psychology, 131, 5-13. https://doi.org/10.1016/j.biopsycho.2017.05.001 Skeaff, C. M., & Miller, J. (2009). Dietary fat and coronary heart disease: Summary of evidence from prospective cohort and randomised controlled trials. Annals of Nutrition & Metabolism, 55(1/3), 173-2001. https://www.jstor.org/stable/48514098 Skodol, A. E. (2010). The resilient personality. In J. W., Reich, A. J. Zautra, J. S. Hall (Eds). Handbook of adult resilience (pp. 112-125). The Guilford Press. Smith, G. D. Ben-Shlomo, Y., Beswick, A., Lightman, S., & Elwood, P. (2005). Cortisol, testosterone, and coronary heart disease. Circulation, 112(3), 332-340. https://doi.org/10.1161/CIRCULATIONAHA.104.489088 Starkman, M. N., Giordani, B., Berent, S., Schork, M., & Schteingart, D. E. (2001). Elevated Cortisol Levels in Cushing’s Disease Are Associated With Cognitive Decrements. Psychosomatic Medicine, 63(6), 985-993. http//www.doi.10.1097/00006842-200111000-00018 Stojanovitch, J., & Marisavljevich, D. (2008). Stress as a trigger of autoimmune disease. Autoimmunity Review, 7(3), 2009-213. 213. https://doi.org/10.1016/j.autrev.2007.11.007 Strickland, B. R. (1989). Internal-locus control expectancies: From contingencies to creativity. American Psychologist, 44, 1-12. https:/doi.org/10.1037/0003-066x.44.1.1 Taylor, S. E., (2009). Health psychology (6th ed.) New York, NY: McGraw-Hill. van Peer, J. M., Roelofs, K., & Spinhoven, P. (2008). Cortisol administration enhances the coupling of midfrontal delta and beta oscillations. International Journal of Psychophysiology, 67(2). 144-150. https://doi.org/10.1016/j.ijpsycho.2007.11.001 Wells, G. (2021). Manage stress to enter into Alpha-Brainwaves. https://drgregwells.com/blog/manage-stress-to-enter-into-alpha-brainwaves Whirledge, S., & Cidlowski, J. A., (2010). Glucocorticoids, stress, and fertility. Endocrinology, 35(2), 109-125. http//doi.10.1210/en.2013-1652 Wingenfeld, K., & Wolf, O. T. Stress, memory, and the hippocampus. Frontiers of Neurology and Neuroscience, 34, 109-120. http//doi.10.1159/000356423
|