|
FOOD PSYCHOLOGY Daniel Roberts, Ph.D. & Brenda MacDonald, M.Ed. |
||||||||||||||||||
|
Fats and Oils Summary. Dietary fats are necessary for good health; however, all fats are not created equal. In fact, some fats have been the source of metabolic disruptions interfering with good heath. Our dietary fats come from different food sources and the list of organ systems and metabolic processes where fatty acids are involved are many. To name a few, fats are a source of energy, required to make hormones, absorb vitamins, and participate in the making of cell membranes, such as those of the lining of the arteries and intestinal tract. Importantly, our brain, which is mostly fat, requires specific fatty acids to function properly: e.g., myelin, which insulate neurons and axons, are made of diverse cholesterol molecules. Cholesterol levels (e.g., omega-3 and omega-6) when off-balance are implicated in a host of metabolic dysfunctions that lead to a multitude of diseases, including diabetes and coronary heart disease. As well, a lack of omega-3 derivative fatty acids (e.g., docosahezaenoic acid: DHA) are associated with physiological pathologies, such as brain dysfunctions and, consequently, cognitive problems: learning and memory impairments as well as mental health issues. Additionally, vitamins and minerals, along with fatty acids, have essential functions in metabolic processes. In other words, food synergy or having the right amount of nutrients play a crucial role in an individual's health. Aside from traditional nutrients (i.e., carbohydrates, proteins, fats, vitamins, and minerals) other food components known as antioxidants which inhibit oxidative stress and, ultimately, cellular and DNA damage, also prevent the surge of disease, and prolong life. With the continuing research on excess dietary fats, high sugar diets, stress, and so on, the question most of us ask is "What is the optimal diet?" Research points out that consuming the right amount of nutrients protects against chronic and degenerative diseases. However, a person's diet changes over time according to several factors, such as age, genes, gender, health, personality type, education, etc. Artificial intelligence (AI) applications have addressed the proper nutrients based on life factors. AI applications also address diet adjustments based on an individual's regular feedback (i.e., mood, cognition, productivity, stress, wellbeing). The purpose of such dietary assessments are not only to update current nutrient intake, but also to provide guidance in lifestyle strategies (e.g., dietary habits, stress management, cognitive restructuring, and so on) geared to maximize an individual's mental and physical health.
Eating habits often go astray when a person is under stress or eating a high-sugar diet. Stress and diets high in sugar content are controllable risk factors for excess weight or obesity which in turn contribute substantially to risk factors for both physical diseases and mental disorders. The same applies to diets rich in fatty substances. In general, a diet rich in animal or processed vegetal fat is negatively correlated with a multitude of ill effects, including cardiovascular diseases and diabetes, as well as degenerative diseases such as dementias. Also impacted are people's social abilities and cognitive skills. Fats and oils are necessary for good health. The list of organ systems and metabolic processes in which fat is needed is vast and complex. We use some fats to make the membranes of cells. We need cholesterol to make certain hormones, to clot our blood and to contract, and relax our blood vessels. We also need fat for proper immune functions. Dietary fat gives us energy and helps our body absorb vitamins. Importantly, for our brain to achieve its optimum level of complexity, and therefore peak performance, it needs saturated fat, polyunsaturated fat, cholesterol, and a number of other fats. Types of Fats and oils: There are four major classes of dietary fat in food. Of primary importance are triglycerides: saturated and unsaturated fats, cholesterol, and trans fat. Only animal products (e.g., butter, cheese, fish and meat) are rich in saturated fats. Unsaturated fats are found in plant foods. Unsaturated fats are classified into monounsaturated fats, and polyunsaturated fats. Trans fats are not occurring naturally: they are manufactured through a process called hydrogenation, during which some fatty acid molecules become rearranged and convert to trans-fatty acids. Triglycerides are transported in blood attached to protein carriers and used by cells for energy formation and tissue maintenance. When evaluating one's blood lipid profile for risk of illnesses (e.g., for heart disease and diabetes), two factors are considered; (1) the total amount of cholesterol/triglycerides circulating in the blood and, (2) the manner in which cholesterol/triglycerides are transported in the bloodstream. Some fatty acids pass through the cells, such as in the intestinal lining, and travel unassisted to the liver; however, larger lipids require the assistance of lipoproteins to be transported in the blood plasma. Cholesterol LDL and HDL Cholesterol is a fat-like substance in the bloodstream. It is classified as a lipid and soluble in fat, as most fats are. About 80 percent of total body cholesterol is manufactured in the liver, while 20 percent comes from dietary sources; mainly from foods of animal origin. Cholesterol is important for the digestive process, the structure of cell membranes and for the manufacture of hormones. Our body makes most of the cholesterol that is needed; however, when the cholesterol ratio is off balance, such as when there is too much of one type of cholesterol circulating in the bloodstream (e.g., when our diet adds more cholesterol than needed) health issues associated with cholesterol occur. Cholesterol levels are indicators of risk for cardiovascular disease. A Lipoprotein analysis breaks down the total cholesterol into its components or, lipoproteins, of which there are three main classes: very-low, low-, and high density lipoproteins. The last two of these lipoproteins carry important implications for heart health. The high low density of the lipoproteins (HDL) allows it to easily attach to the inner wall of the blood vessels, which causes plaques to accumulate within the artery walls. The higher density lipoprotein (LDL) is described as 'garbage collectors' clearing away plaques and other debris as it flows through the bloodstream to the liver where it is then excreted from the body. Both high- and low-density lipoproteins (HDL and LDL) are necessary for health, provided that their ratio is adequate to carry out their metabolic functions. A cholesterol ratio is the ratio obtained by dividing the Total Cholesterol by the HDL (High-Density Lipoproteins) level. For example, having a Total cholesterol level of 162 mg/dL and an HDL level of 44 mg/dL implies a cholesterol ratio of 3.7. The American Heart Association (AHA) recommends keeping the cholesterol ratio below 5. It is generally accepted that a 4.5 or lower ratio (Total cholesterol/HDL cholesterol) is excellent for men, and 4.0 is best for women. The Total cholesterol/HDL ratio gives an estimate of a person’s probability of developing fat-related illnesses. A laboratory blood test or, more specifically a lipoprotein analysis, is used to evaluate one's blood lipid profile (the total amount of specific HDL and LDL and other fats circulating in the bloodstream for risk of developing illnesses, such as cardiovascular diseases, especially atherosclerosis, i.e. the hardening of arteries. See table 1.
Table 1. Classification of serum lipids in adults (mg/dl: milligrams per deciliter.
The average HDL levels in adults are about 45 to 65mg/dl, with women averaging higher than men. The female sex hormone estrogen raises HDL levels, which may explain why premenopausal women are usually protected from heart disease. Studies suggest that HDL levels above 60 protect against heart disease. In other words, if you have a cholesterol reading of 200, with HDL at 80, and LDL at 120, you are considered at low risk for heart disease. However if you have a total cholesterol level well under 200, and your HDL level is under 35, you can still, with other indicators present (e.g., triglycerides and albumin levels), be considered at increased risk for developing coronary heart disease. Triglycerides provide our body with energy, but their main function is to store excess fats for later use. Triglycerides are also known as free fatty acids and, in combination with cholesterol, they accelerate the formation of plaques. Triglycerides (fat molecules) are carried in the bloodstream by very low density lipoprotein (VLDL). When there’s too much cholesterol in the bloodstream, it builds up in the arteries increasing the risk of heart attack or stroke. These fatty acids are found, for example, in poultry skin, lunch meats, and shellfish. However, they are mainly manufactured in the liver from refined sugar, starch, and metabolized alcohol. High intake of ingested alcohol and sugar (honey included) significantly increases triglycerides. As a general rule, one should keep one's triglyceride level below 200 mg/dl. However, some reports indicate triglyceride levels over 100 can be a cause for concern. Albumin levels are also regarded as a measure of health. Albumin is a chemical protein that has many metabolic functions, including the transport of nutrients and removal of oxidative waste, maintenance of cell stability and control of DNA replication. It also carries various substances throughout our body, including hormones, vitamins, and enzymes. Low albumin levels can indicate a problem with the functioning of the liver and/or kidneys. An albumin blood test measures the amount of albumin in our blood. Albumin is a protein made by our liver. The level of albumin is determined by the level of immune/inflammatory proteins. The greater the stress on the immune system, the lower the level of albumin. The reference range for albumin levels in blood is between 3.4 and 5.4 grams per deciliter (mg/dL). A normal reference range for albumin in urine is between 0 and 8 milligrams per deciliter (mg/dL). It should be noted that high albumin levels do not usually indicate a serious cause, dehydration often being one of the main causes of elevated albumin levels. Metabolic syndrome A metabolic syndrome is a cluster of symptoms that include chronic high blood pressure, elevated triglycerides in the blood, lower 'good' cholesterol, and a reduced capacity of the body's cells to respond to insulin, the hormone which promotes the uptake of blood sugar. Another symptom is a marked increase of abdominal fat: i.e., a waist measurement of 35 inches or more in women and 40 inches or more in men: see table 1. A build-up of excess fat triggers genetic changes that result in inflammation.
Table 1. Diagnostic criteria for metabolic syndrome: Metabolic syndrome is a billable/specific ICD-10-CM code: International Classification of Diseases, Tenth Revision
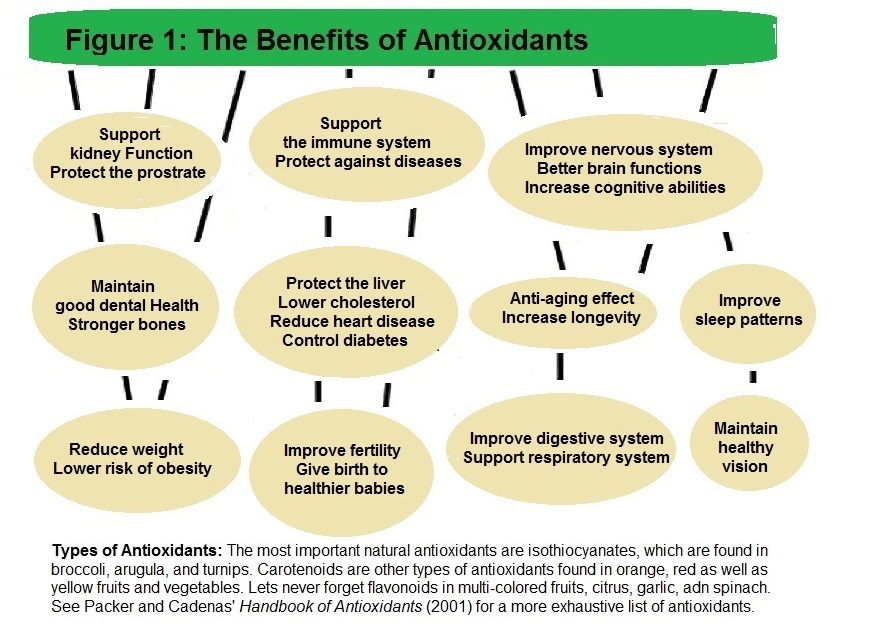
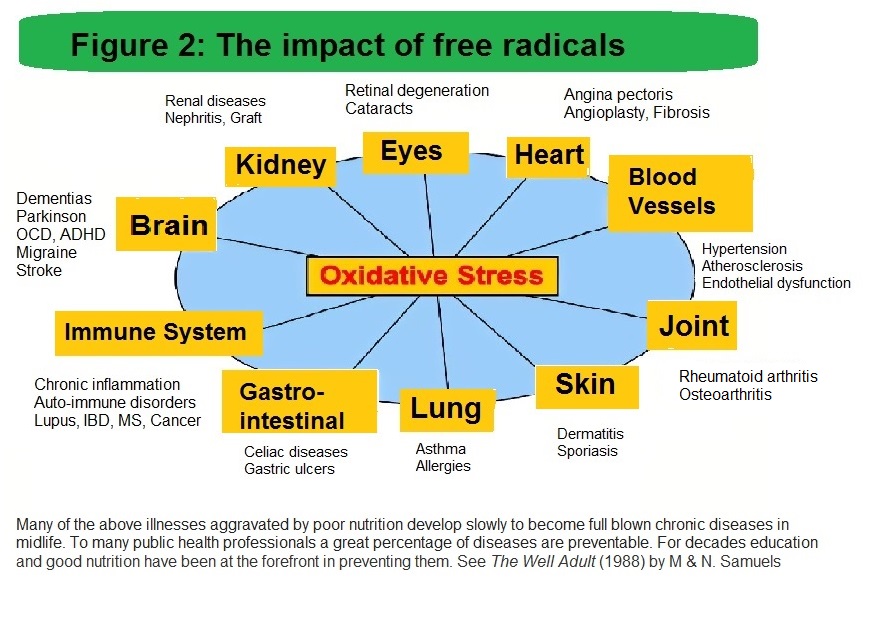
Stored and localized body fat. Recent epidemiological evidence suggests that abdominal fat, as opposed to excessive fat in the hips, buttocks, or thighs, is a risk factor for cardiovascular diseases, diabetes, and cancer. The excess body fat was referred to as 'stress weight' since it increases in response to stress (Rebuffé-Scrive et al., 1992). People with excessive body weight are more reactive to stress and show greater cardiovascular reactivity (Davis et al., 1999) and neuroendocrine reactivity to stress (Epel et al., 2000). Such reactivity to stress linked to fat deposits associated with chronic disease was reported to be a symptom of health erosion in response to stress weight. The stress weight literature points to the importance of maintaining an ideal body weight, as well as a healthy diet, which reduces stress, and the risk of chronic disease that often emerges in middle age. Genetics and cholesterol levels. Genetic differences in how a person metabolizes dietary saturated fat and cholesterol have been related to health. The efficiency at which people process dietary fat is associated with receptors located primarily in liver cells (Brown & Goldstein, 1985). These receptors bind and remove cholesterol from the blood. The more cholesterol receptors an individual has, the more efficiently he/she can remove cholesterol from the blood. The number of cholesterol receptors is genetically determined; however, other factors such as a diet high in triglycerides and lifestyle can influence their number. A diet high in saturated fat increases the risk of disease twofold. It not only saturates the receptors, but also decreases their number. Nonetheless, it is estimated that five (5) percent of the population has a genetically-high cholesterol level that remains elevated regardless of lifestyle. Omega-3 and omega-6 fatty acids Linoleic acid (LA), better known as omega-6s, and alpha-linolenic acid (ALA), known as omega-3s, are two major classes of polyunsaturated fatty acids that promote an individual's general health. About thirty percent of blood cholesterol is carried by HDL. Omega-3s raises HDL levels, while high levels of omega-6s suppresses the uptake of omega-3s into tissues. One fifth (20 %) of our brain fat is composed of essential fatty acids, omega-3 and omega-6. Within this perspective the human brain is, as a whole, nearly sixty (60) percent fat. Omega fatty acids cannot be manufactured within the body; hence, omega-3 and omega-6 are labelled essential and need to be acquired in the diet. Omega-6 fatty acids, such as gamma-linolenic acid (GLA), are required for growth, the maintenance of healthy skin, and normal functioning of the reproductive system. It is a component of all cell membranes and is found in particularly high amounts in nerves and the brain. A number of biologically active compounds produced in the body that participate in regulation of blood pressure and blood clotting are derived from linoleic acids. Omega-6 fatty acids are different from omega-3 fatty acids. The major food source of omega-6s are found in some plant oils and seeds, such as sunflower, safflower, corn, and soybean oil. Omega-3 fatty acids also referred as 'n-3s' participate in the structural component of all cell membranes. N-3s are found in high amounts in the brain and other nervous system tissues, such as in the myelin sheath covering and insulating the nerve cells and axons. They are biologically active compounds used in the regulation of blood pressure and clotting; but these compounds have the opposite effects on blood pressure and blood clotting as do derivatives of linoleic acids. Omega-3 fatty acids are found in walnuts, dark, leafy green vegetables, and flaxseed, canola, and soybean oils in the form of alpha-linolenic acid. Importantly, alpha-linolenic acid (ALA) is converted into eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), which occur primarily in the liver. Their production is limited, with reported rates of about 15 percent. Therefore, consuming EPA and DHA from foods and/or dietary supplements is the way in which one can increase levels of these fatty acids for optimal mind and body functioning. Health benefits of polyunsaturated fats The statistics relating fish consumption to cardiovascular health has been extensively documented. In a study, women who ate fish two to four times a week were 40 percent less likely to suffer a stroke than women who ate very little fish. In another study, men who consumed seven (7) ounces or more of fish per week had a 59 percent lower risk of having a heart attack than men who consumed less than two (2) ounces of fish per week. In addition to reducing the risk of cardiovascular disease, the anti-inflammatory properties of omega-3s have protective effects against illness, such as arthritis, renal dysfunctions, and diabetic nephropathy (Bernasconi et al., 2021; DeFillippis et al., 2010; Köhler et al., 2010). Dietary fats, IQ and cognition Empirical studies point to fatty acid imbalance affecting mental, physical, and emotional intelligence (Horrocks & Yeo, 1999; Schmidt, 2007). Mental intelligence includes cognitive measures associated with IQ, such as verbal and nonverbal intelligence. Omega-3 dietary fatty acids have positive effects on children and older adults' general intelligence as well as their cognitive performance (Lassek & Gaulin, 2011; Theodore et al., 2009). One type of long-chain omega-3 fatty acid, docosahexaenoic acid (DHA), was reported to be essential for the development of normal brain function (Horta et al., 2015; Leino et al., 2013). Some dietary fatty acid imbalance affects academic performance. The assessment of boys' academic skills (math and overall academic ability) was found to be lower in the group with lower omega-3 fatty acids (Kuratko et al., 2013; Stevens et al., 1996). Several studies were conducted with students diagnosed with mild to severe learning disabilities (e.g., dyslexia., nonverbal learning and visual processing disabilities, ADD and ADHD). On average, after one year on DHA (docosahexaenoic acid), students made significant gains. Academically, their marks improved as did their social skills (Garami, Das & Das, 2015; Milte, Parletta, Buckley et al, 2012; Richardson & Puri, 2002; Stordy, 2000). Other studies found a fatty acids imbalance to be associated with short- and long-term memory impairment (Siguel, 1994; Andrurchow et al., 2017). When alpha-linolenic acids (e.g., omega-3 fats such as eicosapentaenoic acid: EPA) was added to correct the fatty acid imbalance, individuals' memory significantly improved. Siguel contends that fatty acids and their derivatives are critical to the nervous system. He also points out that the chronic abnormal levels of omega-3 fatty acids derivatives account for a significant portion of mental and social impairments. Omega-3 fatty acids derivatives are eicosapentaenoic acid (EPA), docosapentaenoic acid (DPA), and docosahexaenoic acid (DHA). Mood and behavior: Several studies have shown fat intake contributes to erratic moods; participants who were on a no-fat diet were more irritable than those on a regular diet. Other studies have associated a low-fat diet, and especially low-cholesterol diets, to behavioral problems (Stevens et al., 1996; Virkkunen et al., 1987). A plausible cause of these effects could be that low-fat diets produce low levels of serotonin in the brain (Muldoon et al., 1992). The most common behavioral difficulties associated with fatty acids imbalance, especially low omega-3 fatty acids, include a domineering attitude, temper tantrums, impulsivity, anxiety, hyperactivity, and conduct problems (Blaun, 1996). Fats and mental health: Low cholesterol levels have has been related to an increase in anxiety and depressive symptoms (Davidson et al, 1996, Maes et al, 1996). Adams et al. (1996) who studied the blood of people with moderate to severe depression found the balance of essential fatty acids was significantly altered; particularly, their level of omega-3 fatty acids was low. Glueck (1994) reported that elevated triglycerides, high total cholesterol, and Low HDL (or low 'good' cholesterol) was the cause of depression in patients being treated for a form of hyperlipidemia. Conversely, Hibbeln & Salem (1995) found that adequate long chain polysaturated fatty acids, particularly DHA, reduce the rate of depression just as omega-3 polyunsaturated fatty acids reduces coronary artery disease. Vitamins and minerals Dietary fats help absorb vitamins; both play a crucial role in the quality of an individual's health. Vitamins are organic substances while minerals (e.g., sodium and calcium) are inorganic substances. Importantly, most vitamins must be obtained from 'natural' food sources. Moreover, each vitamin has specific metabolic functions. Vitamins and minerals complement each other (i.e., work in synergy) having essential functions in metabolic processes. For instance, cells need iron for electron transport chains, and the red blood cells cannot function without iron in haemoglobin (the oxygen-carrying pigment in blood). Vitamins (or phytochemicals) are present in frequently-consumed food like fruit, vegetables (broccoli and kale), grains and legumes (beans and peanuts), nuts (almonds, walnuts, hazelnuts), and seeds (chia, hemp hearts, flaxseed and quinoa). Nuts per se contain high amounts of magnesium, copper, folic acid, potassium, and fiber as well as vitamins A, C and E. Vitamins are also found in garlic, soy and green tea. These plant pigments interact with hormone receptors to suppress malignant changes in cells, increase immune functions, and reduce cholesterol levels. Chronic deficiencies of vitamins and minerals have been associated with at least four of the leading causes of death: cancer, cardiovascular diseases, diabetes, and hypertension (Brown, 2005; Sizer & Whitney, 2006). In addition, vitamins and minerals contribute to cognitive health. It is important to note that excessive toxic levels of some food nutrients (e.g., dietary fats) or micronutrients can cause a host of health problems. A common problem are low-fat diets. A little dietary fat is needed for basic metabolic functions, especially for the absorption of fat-soluble vitamins. A minimum of 15 to 25 grams per day usually satisfies fat requirements. Also, fat is burned more completely in the presence of carbohydrates. The adverse effects of a low-carbohydrate (low glucose availability) and high fat diet include physiologic ketosis. Fats burned for energy in the absence of carbohydrates produces a toxic waste product called ketone bodies. Ketosis, an accumulation of poisonous ketone bodies, causes fatigue and nausea and overtaxes the kidneys, resulting in nerve and brain damage. Other side-effects include headaches as well as cramps, especially in the lower extremities. Common Vitamins: There are two natural basic classes of vitamins; those that are soluble in water (the B-Complex vitamins and vitamin C) and others that dissolve in fat (vitamins D. E, K, and A). Solubility determines how vitamins are absorbed into and transported around the bloodstream, whether they can be stored in the body (as in the liver), and how easily they are excreted from the body. One group of vitamins known as antioxidants (vitamin C, vitamin E, beta-carotene, and selenium, which is plentiful in sardines) have been shown to ward off cardiovascular disease, certain cancers, hypertension, and cataracts. Vitamin A exerts considerable influence on body functions through it's regulation of the activities of the genes (Bastien & Rochette-Egly, 2004; Wei, 2003). Genes direct the synthesis of proteins, including enzymes, and enzymes perform the metabolic work of the tissues. Vitamin A is needed in reactions that generate new cells to replace worn-out cells lining the mouth, oesophagus, intestines and the eyes, especially the maintenance of a healthy, crystal-clear cornea. Without enough vitamin A, old cells are not replaced, and the affected tissues end-up being damaged. Hence, factors that influence gene expressions also affect the metabolic activities of the tissues and, importantly, health. Let us note that vitamin deficiency (avitaminosis) can lead to metabolic problems, as does excess intake of vitamins (i.e., hypervitaminosis). For example, consuming large amount of vitamin A over a three-month period or more can cause dry skin, hair loss, anorexia, and vomiting. Long-term, over-consummation of vitamin A leads to headaches, and mental disturbances, liver enlargement, and occasionally, cirrhosis. Like vitamins, minerals are beneficial only when taken in the proper amounts. For example, an increase in sodium (salt) concentration in the bloodstream can be toxic. It causes hypernatremia, a shrinking of the cells in various body tissues, including those of the brain. Shrinkage of the brain cells results in confusion, coma, paralysis of the lung muscles, and death. As well, high sodium consumption can raise blood pressure, and high blood pressure is a major risk factor for heart disease and stroke. Vitamin D is different from all other nutrients in that the body can synthesize all it needs with the help of sunlight. In northern countries, a vitamin D supplement is recommended because of shorter periods of sunlight during the long winter. Vitamin D is best known as a category of nutrients and hormones that interact to regulate blood calcium and phosphorus levels, thereby maintaining bone integrity. Calcium is indispensable to the proper functioning of cells in all tissues of the body, including muscles, nerves, and glands (Kato, 2000). Research points out that deficiencies of vitamin D lead to health problems, including high blood pressure, diabetes, heart disease, rheumatoid arthritis, osteoporosis, and diseases related to chronic inflammation, such as inflammatory bowel disease (Cantorna et al 2004; Holick, 2004). Vitamin C is required for reactions that build and maintain collagen, a protein found in skin, bones, blood vessels, gums, ligaments, and cartilage. Dr. Linus Pauling (see Higdon & Drake, 2012) place vitamin C at the forefront of antioxidants. Vitamin C protects substances from oxidation by being oxidized itself. For example, cells of the immune system maintain high levels of vitamin C to protect themselves from free radicals generated from bacterial infections (Padayatty et al., 2003). Studies of vitamin C suggest that it can help prevent cancer, lower the risk of cardiovascular disease and improve arthritis. Fresh fruits and vegetables are foods rich in Vitamin C, Vitamin E is considered an anti-aging antioxidant that improves the immune system, protects against sun damage, relieves arthritic symptoms, and makes strong cell walls. Vitamin E is a fat soluble antioxidant which breaks the chain of free radicals acting on lipids, and preventing free radicals from damaging lipids and proteins. Free radicals, formed during normal cell metabolism, were reported to play a role in the development of some types of cancer, bronchitis, emphysema, heart disease, cataracts, and premature aging (Johnston & Corte, 1999). Food sources of vitamin C and E are associated with slowed progression of Alzheimer's disease, reduced plaque formation in the arteries, and improved circulation in patients with diabetes (Halvorsen et al, 2006). Vitamin K. The main function of vitamin K is to help synthesize proteins that help clot the blood, such as when an injury occurs on the lining of a blood vessel. Vitamin K deficiencies does not improve clotting in people with bleeding disorders as in the inherited disease haemophilia. However, the counter action of vitamin K is desirable for individuals with heart problems (e.g., atrial fibrillation) who need to take blood thinning medication to prevent the formation of clots within their circulatory system, and to avoid stroke, such as that in the brain, which can be fatal. Vitamin K has a multitude of other functions. In combination with vitamin D, it ensures the health of the bones, reducing the risk of hip fracture. Vitamin K also promotes cognitive health. In one study, healthy individuals over the age of 70 years with the highest blood levels of vitamin K1 had the highest verbal episodic memory performance. Generally, vitamin K has been shown to improve cognitive and psychological functions, especially in aging (Bolzetta et al., 2019; Kiely et al., 2018; Lin et al, 2021). Vitamin K can be obtained from the gut intestinal bacteria. Plant food sources that are rich in vitamin K include dark green leafy vegetables such spinach and collard greens, broccoli, and brussels sprouts. Vitamins B. Each and every vitamin B is involved in energy metabolism; a lack of it manifest itself in low energy and a multitude of other symptoms. The symptoms of B vitamin deficiencies and toxicities (when taken in large amounts) include an enlarged heart, abnormal heart rhythms, heart failure, loss of reflexes, forgetfulness and mental confusion, skin rash, muscle pain, impairment of the immune response and damage to the digestive system. Significant sources of B vitamins are whole and enriched grains, legumes, seeds, vegetables and moderate amounts of meat, such as pork, and liver. Of the B vitamins, vitamin B12 helps cells to multiply, which is especially important for cells with a shorter life span. Such cells include red blood cells (which live for about 120 days) and the cells that line the digestive track (which are replaced every three days). Vitamin B12's other functions are to help maintain the sheath that surrounds and protects nerve fibers (i.e., the myelin). A lack of vitamin B12 will compromise this protective function and lead to damaged nerve sheaths, as well as malfunctioning of the nerves and muscles. Sources of Vitamin B12. are foods of animal origin, including fish, meat, poultry, eggs, and dairy products.. It is recommended that a strict vegetarian takes B12 vitamin supplements as lack of it will cause ill effects, such as anaemia, chronic fatigue and insomnia. Thiamin and Riboflavin (vitamins B1 and B2). Thiamin or thiamine also participate in the energy metabolism of all cells, including muscle and nerve cells. A classic thiamin-deficiency disease is beriberi, once caused by removing the rice's brown coat, which contains thiamin. Alcohol abuse often leads to a severe form of thiamin deficiency; e.g., the Wernicke-Korsakoff syndrome. Thiamin occurs in small amounts in many nutritious foods, including sunflower seeds, enriched or whole-grain cereals, and legumes. Niacin (vitamin B3). The vitamin niacin, like thiamin and roboflavin, participate in the energy metabolism of every cell of the body. A well-known niacin-deficiency disease is pellagra. Its symptoms are known as the four Ds: diarrhea, dermatitis, dementia, and death. Genetic engineering (GM) was used to improve corn (or maize) nutrients and reduce the risk of pellagra. This process has led to several transgenic plants to produce more total starch, protein, nitrogen, and essential amino acids in the seeds, thus improving people's general health, and cognition. Another example is golden rice, genetically modified to accelerate the synthesis of vitamin A, which may be helpful in developing countries where people do not have access to a balanced diet. Folate (vitamin B9) or folic acid (its synthetic form). Folate participates it the making of new cells. More specifically, folate helps to synthesize DNA. Folate deficiency is associated with birth defects know as neural tube defects, causing spine problems, diminished brain size, and mental retardation. One of the causes is pregnant mothers' eating too few fruits and vegetables. Research suggests that a diet deficient in folate can also elevate risk of cardiovascular disease and cancer of the colon, and increase women's risk for cervical cancer (Bailey, Rampersaud, & Kauwell, 2003). Phytochemicals vs. antioxidants The food components known as phytochemicals or phytonutrients are present in frequently-consumed food such as fruits, vegetables, grains, legumes, and seeds. Phytochemicals have been associated with the prevention and treatment of at least four of the leading causes of death in the US and Canada: cancer, cardiovascular diseases, diabetes, and hypertension (Bryce, 2008). The benefit of phytonutrients is that they also ward off inflammation in the body, preventing tissue damage to the brain, arteries, and joints. On average, Health Canada and the US Food and Drug Administration (FDA) recommends two (2) cups of fruit and three (3) cups of vegetables per day, with one (1) cup of vegetables eaten raw. Antioxidants are molecules that neutralizes free radicals. Free radicals are the by-products of normal metabolism and the inflammation process. Exposure to toxins in the environment, such as polluted soil and air, toxic chemicals, radiation, ultraviolet rays, and tobacco smoke also result in the formation of free radicals. On the molecular level, free radicals are unstable; they each contain an unpaired electron that, in attempts to pair up and stabilize the substance, will bind and take electrons from other substances, including healthy cells. The result is that damaged cells and tissues lead to other healthy cells being damaged. This process, known as oxidative stress damage, leads to cellular destruction and mutations in the body's cells, causing 'cell starvation', and the body's inability to fight off disease. Interestingly, people who live to be centenarians (age 100 or older) have higher levels of antioxidants than individuals with a shorter life span. There are a number of antioxidants and foods high in antioxidants (e.g., wild blueberries, red kidneys beans, pecans, cranberries, strawberries, and dark leafy greens). Dr. Packer described five pivotal antioxidants, which he calls network antioxidants: Apha-lipoic Acid (ALA), coenzime Q10, vitamin C, the natural form of vitamin E, and glutahione. Packer concluded that the synergy among these antioxidants slow aging and, most importantly, prevent and slow diseases (Packer, 2019; Imirit, Packer & Auclair, 2012; Packer & Prilipko, 2011).
Most research studies have established a strong link between inflammation and chronic conditions like cancer, autoimmune disease, lung and heart disease, gut disorders, asthma, and diabetes. Antioxidants like carotenoids and flavonoids, which give fruits and vegetables their bright color, help reduce the body's inflammatory response caused by free radicals. Anything that reduces oxidation reduces inflammation, and anything that reduces inflammation reduces oxidation. So, it is often highly recommended that food rich in antioxidants be part of one's diet to prevent chronic disease. Nonetheless, westerners consume minimal amounts if none of these foods, which is said to partly explain the rise of chronic diseases. Actually, the trend among westerners is to eat food categories rich in unhealthy fats and sugars, which has caused the rise of chronic diseases.
Coronary heart disease Research has linked high levels of cholesterol and other blood fats as well as free radicals to the onset and the progression of cardiovascular disease (CVD). Often affected are the blood vessels, especially the coronary arteries. Arteries have a thin layer of endothelial cells that degrade as a result of arteriosclerosis; i.e., the thickening and hardening of the arteries. It is a progressive condition in which deposits of cholesterol and other lipids (e.g., HDL), with cellular waste products (i.e., the build-up of plaques) accumulate on the inner walls of damaged arteries. As the build-up of plaques progress, blood vessels lose their elasticity and become clogged. A blood clot may form on the plaque build-up and block the entire artery, such as in the case of myocardial infarction, or heart attack, and stroke. Vulnerability to cardiovascular disease is influenced by other dietary factors, such as a low-fibre diet (Fung, 2016; Ludwig et al., 1999), and high intake of red meats, potatoes, and refined grain (Hu & Willert, 2002). Changes in the environment because of migration to different geographic locations, modifications in lifestyle choices, and shifts in social policies and cultural practices alter CVD risk, even in the absence of genetic changes. On the subject of red meat, a distinction is warranted as to the type of animal fat that is more likely to cause chronic disease. Research points to red meat containing various types of fat—not only saturated fat, but also omega-6 fat (found in high amounts in corn-fed feed lot cows) and omega-3 fat (found in grain-fed meat). Omega-rich food like nuts, seeds, and fatty fish also have essential fatty acids. Either way, these fatty acids, and essential fatty acids, linked to prevention of degenerative conditions, must come from our diet. Vanderhaeghe and Karst (2004) research showed that certain types of essential fatty acids (EFAs)—healthy fats—improve immune and hormone functions, and play a vital role in preventing and treating all forms of degenerative disease, including CVD, brain related disease, and cancer. Myelin and brain disorders All oils are not created equal; there are healthy fats, fats that can damage the arteries, and other fats providing essential food nutrients to all body organs, including cells, and our brain. A lack of essential fatty acids to our brain correlates with physiological pathologies, such brain dysfunctions, and consequently, cognitive problems: impairment in learning, memory, concentration and attention, etc. Rudin and Felix (1996) has linked fatty acid imbalance to a number of psychological conditions, as did many other researchers who produced noteworthy work on the subject of fatty acids and brain disorders (see Hibbeln & Salem, 1995; Mitchell et al, 1987; Nagy & Tiuca, 2017; Newton, 2001). Myelin is primarily affected by lack of proper fatty acids. The basic function of myelin is to speed the transmission of nerve impulses; thus, making nerve transmission more efficient and rapid. Myelin is made of various fats, fatty acids, phospholipids, cholesterol, and proteins. Formation of myelin is highly dependent upon nutritional intake because some fatty acids cannot be manufactured by the body. They must be obtained from the food we eat. Though the actual fatty acids are slightly different, the need for an omega-6 and omega-3 proper ratio is important. As pointed out previously, a fatty acid imbalance sets the stage for poor structural tone and artery wall damage. Research on the myelin sheath has been conclusive; not only does a fatty acid imbalance but also a vitamin B12 deficiency affects the myelin sheath. Vitamin B12 is a fat-soluble vitamin that plays a role in fat and protein metabolism, red blood cell production and normal nerve function. A lack of essential fatty acids and vitamin B12 restricts nerve impulse velocity, leading to motor weakness. It leads to loss of myelin (or demyelinating disorders) including sensory impairment, such as blurred vision, difficulties in controlling movement, and problems with bodily functions, such as incontinence. The most common disease associated with myelin damage is multiple sclerosis (MS), where the immune cells attack myelin—and eventually, the nerve axons—in the brain and spinal cord. In addition, loss of the myelin sheath has shown to have adverse effects on cognitive health. A person affected with a demyelinating disorder may experience depression, anxiety, irritability, and problems with thinking, memory, and focus. An experiment found rats that were housed in an enriched environment had more myelin on their axons than rats housed in a dull environment. Rats with more myelin sheath also performed significantly better in mazes. Other studies with humans have shown that environmental enrichment consisting of increased physical, intellectual, and social activity has wide-ranging effects, including enhanced cognition, learning and memory, and motor coordination (Punic, Punic & Kraig, 2016; Thamizhoviya & Vanisree, 2021). Animal studies: DHA and vitamin B3 A great number of animal studies point to fatty acid deficiencies leading to an array of dysfunctional behavior. Interestingly, supplementation of fatty acids, especially with docosahezaenoic acid (DHA) has been shown to significantly improve both animal learning and behavior. Vitamin deficiencies and supplementation of vitamins have similar effects, improving both learning and social behavior. For instance, Yokota (1993) had animals consuming low amounts of omega-fatty acids which caused them to have difficulty learning to avoid a threatening situation. However, adequate amounts of omega-3 led to higher rates of learning. Rats in the high omega-3 fatty acid group were 100 percent successful after only three or four attempts. On the other hand, the group fed a low omega-3 diet was only thirty to forty percent successful even after the twentieth attempt. The authors concluded that this indicated that a deficiency of the brain DHA level resulted in a reduction of learning ability. Greenwood and Winocur's (1996) studies looked at the effect fat had on memory and performance. Some animals were fed a diet in which they receive 10 percent of their calories from fat, while others received forty percent of their calories from fat. The remainder were fed between ten to forty percent fat diets. Forty percent is similar to the fat content of the standard North American diet. The results show that animals who were fed the high-saturated-fat diet had the lowest performance on memory tests. Those fed the diets lowest in saturated fat did best. Of importance is a study done with the wild European hamster that used to thrive in the plains of France's Alsace region. Since the 1960s, their population has declined and was almost the verge of extinction. Tissier et al. (2016) linked the wild hamster decline to maize-based diets that led to the death of hundreds of thousands of people from pellagra caused by tryptophan and vitamin B3 deficiencies. Tissier's lab experiment consisted of feeding the wild hamsters exclusively with monoculture corn. The results show that during breeding, these hamsters were overly aggressive and sensitive to noise. Most surprisingly, 80 percent of the female hamsters devoured their young the first day after birth. Vitamin B3 supplementation effectively restored reproductive success in maize-fed females. GMO foods to superfoods Since GMO foods were introduced in the 1990s, a recurrent question is whether GMO foods are as healthful and safe to eat as their non-GMO counterparts. The research literature indicates that GMO plants have actually been modified to improve their nutritional value. An example is GMO soybeans, modified to produce healthier oils that can replace trans fat. However, several studies of fruit, vegetables and grains have suggested a decline in nutritional value over time due to soil depletion, and changes in the choice of varieties to be cultivated, with some high-yielding plants being less nutritious than historical varieties. A remedy to this is the quest to develop GMO foods with higher nutritional value or other useful traits to enhance human health; that is, 'superfoods' that reduce the risk of chronic disease, boost testosterone secretion, immunity, and wellbeing as well as increase brain power, motivation, and human productivity. The optimal diet Most food nutritionists and diet therapists consider a healthy diet to consist of six (6) essential nutrients required by the body for optimal health: i.e., carbohydrates, dietary fats, high quality proteins, vitamins, minerals, and water. These nutrients are classified into two categories: macronutrients and micronutrients. Macronutrients are the primary dietary nutrients and include carbohydrates, proteins and fats. Micronutrients refer to vitamins and minerals; i.e., a smaller category of nutrients that do not contain calories and are required in smaller amounts than macronutrients. Most importantly, research points out that our organism needs the right nutrients in different amounts, preferably at every meal and every day. For instance, carbohydrates are best processed in the presence of dietary fats. Dietary fats are necessary for transporting fat-soluble vitamins in the body. What is important is not just the amount of the nutrients required, but also their quality which is vital to healthy development, disease prevention, and overall wellbeing (Fung et al., 2001: Mahan & Arlin, 1992; Ludwig et al, 1999). Artificial Intelligence (AI) applications An important factor to consider is the idea that 'one-diet-fits-all' is not suitable for all. In fact, current research points to diets being tailored to fit an individual's specific needs. The idea is that optimal nutrient intake is determined by a number of factors, some of the most important being a person's age, genetics, gender, personality type and taste preference, health status, environmental temperature, weight, profession and physical activity. Another factor is how nutritional intake helps an individual perform throughout the day; e.g., mood, cognition, stress level, wellbeing, productivity, and so on. Artificial Intelligence (AI) applications have addressed proper nutrient intake based on the above factors. AI applications, available on mobile devices, not only assess diet and updated nutrient intake based on feedback, but also provide guidance in lifestyle strategies (e.g., dietary habits, stress management, cognitive restructuring, and so on) geared to maximize an individual's mental and physical health (Braga et al., 2021; de Moraes Lopes et al., 2020; Lu et al., 2019; Sak & Suchodoiska, 2021). AI applications that guide nutrient intake and lifestyle programs and interventions are regarded as the treatment of choice in the prevention or the treatment of chronic disease, such as obesity, diabetes, and cardiovascular disease (Krittanawong. 2017; Oka, Nomura, Yasugi et al., 2019; Stein & Brooks, 2017). References Adams, P. B., Lawson, S., Sanigorski, A., & Sinclair, A. J. (1996). Arachidonic acid to eicosapentaenoic acid ratio in blood correlates positively with clinical symptoms of depression. Lipids, 31(1), S157-S161. https://doi.org/10.1007/BF02637069 Andruchow, N. D., Konishi, K., Shatenstein, B., & Bohbot, V. D. (2017). A lower ratio of omega-6 to omega-3 fatty acids predicts better hippocampus-dependent spatial memory and cognitive status in older adults. Neuropsychology, 31(7), 724–734. https://doi.org/10.1037/neu0000373 Bailey, L. B., Rampersaud, G. C., & Kauwell, G. P.A. (2003). Folic acid supplement and fortification affect the risk of neural tube defects, vascular disease and cancer: Evolving Science. The Journal of Nutrition, 133(6), 1961S-1968S. https://doi.org/10.1093/jn/133.6.1961S Bastien, J. & Rochette-Egly. (2004). Nuclear retinoid receptors and the transcription of retinoid-target. Genes, 328, 1-16. https://doi.org/10.1016/j.gene.2003.12.005 Bernasconi, A. A., Wiest, M. M., Lavie, C. J., Milani, R. V., & Laukkanen, J. A. (2021). Effect of Omega-3 Dosage on Cardiovascular Outcomes: An Updated Meta-Analysis and Meta-Regression of Interventional Trials. Mayo Clinic Proceedings, 96(2), 304-313. https://doi.org/10.1016/j.mayocp.2020.08.034 Blaun, R. Psychology Today, May/June, 1996: 35-43. Block, A., & Thomson, C. A. (1995). Position of The American Dietetic Association: Phytochemicals and functional foods. Journal of the American Dietetic Association, 95(4), 493. 496. DOI:10.1016/s0002-8223(95)00130-1 Bolzetta, F., Veronese, N., Stubbs, N., et al. (2019). The Relationship between Dietary Vitamin K and Depressive Symptoms in Late Adulthood: A Cross-Sectional Analysis from a Large Cohort Study. Nutrients,11(4), 787. https://doi.org/10.3390/nu11040787 Braga, B. C., Aberman, N. L., Arrieta, A., et al., (2021). Designed of a mobile phone-based artificial intelligence (AI) to assess dietary intake and provide nudges to improve health eating behavior. International Food Policy Research. IFPRI discussion paper. Brown, J. E. (2005). Nutrition Now (5th Ed.). Thomson Wadsworth.. Brown, M. S., & Goldstein, J. L. (1985). The Nobel Prize in Physiology or Medicine 1985 was awarded jointly to Michael S. Brown and Joseph L. Goldstein "for their discoveries concerning the regulation of cholesterol metabolism." https://www.nobelprize.org/prizes/medicine/1985/press-release/ Bryce, W. (2008). The antioxidant prescription: How to use the power of antioxidants to prevent disease and stay healthy for life. Random House Canada. Cantorna, M. T., Zhu, Y., Froicu, M., & Wittke, A. (2004). Vitamin D status. 1, 25-dihydroxyviatman D3 and the immune system. American Journal of Clinical Nutrition, 80(6), 1777S, 1720S. https://doi.org/10.1093/ajcn/80.6.1717S Davidson, K. W., Reddy, S., McGrath, P., Zitner, D., & Mackeen, W. (1996). Increases in depression after cholesterol-lowering drug treatment. Behavioral Medicine, 22(2), 82-84, https://doi.org/10.1080/08964289.1996.9933768 Davis, M. C., Twamley, E. W., Hamilton, N. A., & Sean, P. D. (1999). Body fat distribution and hemodynamic stress responses in premenopausal obese women: A preliminary study. Health Psychology, 18(6), 625-633. https://doi.org/10.1037/0278-6133.18.6.625 de Moraes Lopes, M. H. B., Ferreira, M., Ferreira, A. C. B., et al (2020). Use of artificial intelligence in precision nutrition and fitness.). In artificial intelligence in precision health: From concepts to applications. (Chapter, 20, pp. 465-496). https://doi.org/10.1016/B978-0-12-817133-2.00020-3 DeFilippis, A. P., Blaha, M. J., & Jacobson, T. A. (2010). Omega-3 Fatty Acids for Cardiovascular Disease Prevention. Current Treatment Options in Cardiovascular Medicine, 12, 365-380. https://doi.org/10.1007/s11936-010-0079-4 Emerit, I., Packer, L., & Auclair, C. (2012). Antioxidants in therapy and preventive medicine. Springer. Epel, E. S., McEven, B., Seeman, T. et al. (2000). Stress and body shape: Stress-induced cortisol secretion is consistently greater among women with central fat. Psychosomatic Medicine, 62(5),623-632. https://doi.org/10.1097/00006842-200009000-00005 Fung, J. (2016). The obesity code: Unlocking the Secrets of Weight Loss. Greystone books.Fung, T. T., Willett, W. C., Stampfer, M. J., Manson J. E., & Hu, F. B. (2001). Archives of Internal Medicine. doi:10.1001/archinte.161.15.1857 Gharami, K., Das, M., & Das, S. (2015). Essential role of docosahexaenoic acid towards development of a smarter brain. Neurochemistry International, 89, 51-62. https://doi.org/10.1016/j.neuint.2015.08.014 Glueck, C. J., Tieger, M., Kunkel, R., et al. Improvement in symptoms of depression and in an index of life stressor accompany treatment of severe hypertriglyceridemia. Biological Psychiatry, 34(4), 240-252. https://doi.org/10.1016/0006-3223(93)90078-r Greenwood, C. E., & Winocur, G. (1996). Cognitive impairment in rats fed high-fat diets: A specific effect of saturated fatty-acid intake. Behavioral Neuroscience, 110(3), 451–459. https://doi.org/10.1037/0735-7044.110.3.451 Halvorsen, B. L., Carlsen, M. H., Phillips, K. M., et al. (2006). Content of redox-active compounds (i.e., antioxidants) in foods consumed it he United States. American Journal of Clinical Nutrition, 84, 95-135. https://doi.org/10.1093/ajcn/84.1.95 Hibbeln, J. R., & Salem Jr., N. (1995). Dietary polyunsaturated fatty acids and depression: when cholesterol does not satisfy. American Journal of Clinical Nutrition, 62(1), 1-9. https://doi.org/10.1093/ajcn/62.1.1 Higdon, J. (2007). An evidence-based approach of phytochemicals and other dietary factors. Thieme Medical Publishers inc. Holick, M. F. (2004). Vitamin D: Importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis. American Journal of Clinical Nutrition. 79(3), 362-371. https://doi.org/10.1093/ajcn/79.3.362 Horrocks, L. A., & Yeo, Y. K. (1999) Health benefits of docosahexaenoic acid (DHA). Pharmacological Research, 40(3), 211-255. https://doi.org/10.1006/phrs.1999.0495 Horta, B. L., Loret de Mola, C., & Victora, C. G. (2015). Breastfeeding and intelligence: a systematic review and meta-analysis Acta Paediatrica, 103 (S467). https://doi.org/10.1111/apa.13139 Hu, F. B., & Willett, W.C. (2002). Optimal diets for prevention of coronary heart disease. JAMA, 288(20), 2569-78. https://doi.org/10.1001/jama.288.20.2569 Johnston, C. S., & Corte, C. (1999). People with marginal vitamin C status are at high risk of developing vitamin C deficiency. Journal of the American Dietetic Association. 99, 854-856. DOI:10.1016/S0002-8223(99)00203-5 Kato, S. (2000). Molecular mechanism of transcriptional control by nuclear vitamin receptors. British Journal in Nutrition, 84(S2), S229-S233. https://doi.org/10.1079/09658219738859 Kiely, A., Ferland, G. Ouliass, B., O'Toole, P. W., Purtill, H., & O'Conners E. M. (2018). Vitamin K status and inflammation are associated with cognition in older Irish adults. 591-599. https://doi.org/10.1080/1028415X.2018.1536411 Köhler, A., Bittner, D. L., Löw, A., & von Schacy, C. (2010). Effects of a convenience drink fortified with n-3 fatty acids on the n-3 index. British Journal of Nutrition, 104(5), 729-736. https://doi.org/10.1017/S0007114510001054 Krittanawong, C., Zhang, H., Wang, Z., Aydar, M., & Kitai, T. (2017). Artificial Intelligence in Precision Cardiovascular Medicine. Journal of the American College of Cardiology, 69(21) 2657–2664. https://doi.org/10.1016/j.jacc.2017.03.571 Kuratko, C. N., Cernkovitch-Barrett, E., Nelson, E. B., & Salem, Jr., N. (2013). The Relationship of Docosahexaenoic Acid (DHA) with Learning and Behavior in Healthy Children: A Review. Nutrients, 5(7), 2777-2810. https://doi.org/10.3390/nu5072777 Lassek, W. D., & Gaulin, S. J. C. (2011). Sex differences in the relationship of dietary fatty acids to cognitive measures in American children. Frontiers in Evolutionary Neuroscience. https://doi.org/10.3389/fnevo.2011.00005 Leino, O., Karjalainen, A. K., & Tuomisto, J. T. (2013). Effects of docosahexaenoic acid and methylmercury on child’s brain development due to consumption of fish by Finnish mother during pregnancy: A probabilistic modeling approach. Food and Chemical Toxicology, 54, 50-58. https://doi.org/10.1016/j.fct.2011.06.052t Lin, X., Wen, X,, Wei, Z., et al. (2021). Vitamin K2 protects against Aβ42-induced neurotoxicity by activation autophagy and improving mitochondiral functions in Drosophilia. Neuroreport, 32(6), 431-437. 10.1097/WNR.0000000000001599 Lu, Y., Stathopoulou, T., Vasiloglou, M. F., Christodoulidis, S., & Stanga, Z. (2019). An Artificial Intelligence-Based System to Assess Nutrient Intake for Hospitalised Patients. 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC). 10.1109/EMBC43219.2019 Ludwig, D. S., Maizoub, J. A., Al-Zahrani, A., et al. (1999). High Glycemic Index Foods, Overeating, and Obesity, Pediatrics, 103(3), e26. https://doi.org/10.1542/peds.103.3.e26 Maes, M., Smith, R., Christophe, A., Cosyns, P., Desnyder, R. & Meltzer, H. (1996). Fatty acid composition in major depression: decreased omega 3 fractions in cholesteryl esters and increased C20: 4 omega 6/C20:5 omega 3 ratio in cholesteryl esters and phospholipids. Journal of Affective Disorders, 38(1), 35-46. 10.1016/0165-0327(95)00092-5 Mahan, L. K., & Arlin, M. T. (1992). Krause's food nutrition & diet therapy (8th Edition). W. B. Saunders Company. McNamara RK, Able J, Jandacek R. (2020). Docosahexaenoic acid supplementation increases prefrontal cortex activation during sustained attention in healthy boys: a placebo-controlled, dose-ranging, functional magnetic resonance imaging study. American Journal of Clinical Nutrition, 91(4),1060–1067. https://doi: 10.3945/ajcn.2009.28549 Milte, C. M., Parletta, N., Buckley, J. D., et al. (2012). Eicosapentaenoic and docosahexaenoic acids, cognition, and behavior in children with attention-deficit/hyperactivity disorder: A randomized controlled trial. Nutrition, 28(6), 670-677. https://doi.org/10.1016/j.nut.2011.12.009 Mitchell, E. A., Aman, M. G., Turbott, S. H., & Manku, M. (1987). Clinical characteristics and serum essential fatty acids levels in hyperactive children, Clinical Pediatrics, 26, 406-411. https://doi.org/10.1177/000992288702600805 Muldoon, M. F., Kaplan, J. R., Manuck, S. B., & Mann, J. J. (1992). Effects of a low-fat diet on brain serotonergic responsivity in cynomolgus monkeys. Biological Psychiatry, 31(7), 739–742. https://doi.org/10.1016/0006-3223(92)90285-8 Nagy, L., & Tiuca, L.-D. (2017). Importance of fatty acids in physiopathology of human body. In A. Catala (ed.). Fatty acids (Chap. 1). DOI: 10.5772/67407 Newton, I. S. (2001). Long-chain fatty acids in health and nutrition. In F. Shahidi & J. W. Finley (Eds). Omega-3 fatty acids: Chemistry, Nutrition, and Health Effects (Chap. 2, pp. 14-27). ACS Publications. DOI:10.1021/bk-2001-0788.ch002 Oka, R., Nomura, A., Yasugi, A., et al. (2019). Study protocol for the effects of artificial intelligence (AI)-supported automated nutritional intervention on glycemic control in patients with Type 2 diabetes Mellitus. Diabetes Therapy, 10,1151–1161 (2019). https://doi.org/10.1007/s13300-019-0595-5 Packer, L. (2019). Vitamin E in health and disease: Biochemistry and clinical application. Packer, L., & Cadenas, E. (2001). Handbook of antioxidants (2nd edition). Marcel Dekker, Inc. Packer, L., & Prilipko, L. (2011). Free radicals in the brain: Aging, neurological and mental disorders. Springer. Padayatty, S. J., Katz, A., Wang, Y., et al,. (2003). Vitamin C as an antioxidant: Evaluation in disease prevention. Journal of the American College of Nutrition, 22, 18-35. https://doi.org/10.1080/07315724.2003.10719272 Punic, K. M., Pusic, A. D., & Kraig, R. P. (2016). Environmental enrichment stimulates immune cell secretion of exosomes that promote CNS myelination and may regulate Inflammation. Cellular and Molecular Neurobiology, 36, 313–325. https://doi.org/10.1007/s10571-015-0269-4 Rebuffé-Scrive, M., Walsh, U. S., McEven, B., & Rodin, J. R. (1992). Effect of chronic stress and exogenous glucocorticoids on regional fat distribution and metabolism. Physiology and Behavior, 52(3), 583-590. https://doi.org/10.1016/0031-9384(92)90351-2 Richardson, A. J., & Puri, B. K. (2002). A randomized double-blind, placebo-controlled study of the effects of supplementation with highly unsaturated fatty acids on ADHD-related symptoms in children with specific learning difficulties. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 26(2), 233-239 . https://doi.org/10.1016/S0278-5846(01)00254-8 Rudin, D., & Felix, C. (1996). Omega3 oils. Penguin Putnam Inc. Sak, J., & Suchodoiska, M. (2021). Artificial Intelligence in Nutrients Science Research: A Review. Nutrients, 13(2), 322. https://doi.org/10.3390/nu13020322 Samuels, M., & Samuels, N. (1998). The well adult. Summit books. Schmidt, M. A. (2007). Brain-building nutrition: How dietary fats and oils affect mental, physical and emotional intelligence (3rd ed). Berkely, CA: Frog Books. Siguel, E. N. (1994), Essential fatty acids in health and disease. Brookline, Massachusetts: Nutrek press. Sizer, F., & Whitney, E. (2006). Nutrition: Concepts and controversies (10th Ed.). Thomson learning, Inc. Stein, N., & Brooks, K. (2017). A fully automated conversational artificial intelligence for weight loss: longitudinal observational study among overweight and obese adults, JMIR Publications, 2(2). https://doi.org/10.2196/diabetes.8590 Stevens, L. J., Zentall, S. L., Abate, M. L., Kuczek, T., & Burgess, J. R. (1996). Omega-3 fatty acids in boys with behavior, learning, and health problems. Physiology Behavior, 59(4-5), 915-20. DOI:10.1016/0031-9384(95)02207-4 Stevens, L. J., Zentall, S. S., Abate, M. L., Kuczek, T., & Burgess, J. R. (1996). Omega-3 fatty acids in boys with behavior, learning, and health problems. Physiology & Behavior, 59(4-5), 915-929. https://doi.org/10.1016/0031-9384(95)02207-4 Stordy, J. J. (2000). Dark adaptation, motor skills, docosahexaenoic acid, and dyslexia. The American Journal of Clinical Nutrition, 71(1), 323S–326S. https://doi.org/10.1093/ajcn/71.1.323S Thamizhoviya, G., & Vanisree, A. J. (2021). Enriched environment enhances the myelin regulatory factor by mTOR signaling and protects the myelin membrane against oxidative damage in rats exposed to chronic Immobilization stress. Neurochemical Research, 46(12):3314-3324. https://doi.org/10.1007/s11064-021-03433-8 Theodore, R. F., Thompson, J. M. D., Waldie, K. E., et al. (2009). Dietary patterns and intelligence in early and middle childhood. Intelligence, 37(5), 506-513. https://doi.org/10.1016/j.intell.2009.07.001 Tissier, M. L., Handrich, Y., Dallongeville, O., Robin, J.-P., & Habold, C. (2017). Diets derived from maize monoculture cause maternal infanticides in the endangered European hamster due to a vitamin B3 deficiency. Proceedings of the Royal Society B. https://doi.org/10.1098/rspb.2016.2168 Vanderhaeghe, L. R., & Karst, K. (2004). Healthy fats for life: Preventing and treating common health problems with essential fatty acids. Wiley. Virkkunen M. E., Horrobin, D. F., Jenkins, D. K., & Manku, M. S. (1987). Plasma phospholipid essential fatty acids and prostaglandins in alcoholic, habitually violent, and impulsive offenders. Biological Psychiatry, 22(9), 1087-1096. https://doi.org/10.1016/0006-3223(87)90051-5 Wei, L.-N. (2003). Retinoid receptors and their coregulators. Annual Review of Pharmacology and Toxicology, 43(1), 47-72. 10.1146/annurev.pharmtox.43.100901.140301 Yokota, A. (1993). Relationship of polyunsaturated fatty acid (PUFA) and learning ability in the brain of rat fetus and newborn. Nihon Sanka Fujinka Gakkay Zasshi; 45(1), 15-22
|
||||||||||||||||||